Understanding Nonverbality Through
Speech-Motor Pathways
Understanding Nonverbality Through Speech-Motor Pathways
The term apraxia of speech is commonly used to describe difficulty coordinating speech movements, but most discussions stop at the behavioral level. What is missing is the mechanistic explanation of how speech is physically produced.
Speech does not originate in the brain.
The brain does not “speak.”
The brain generates the intention to communicate, but speech itself is the result of physical motor execution in the face, larynx, and vocal tract.
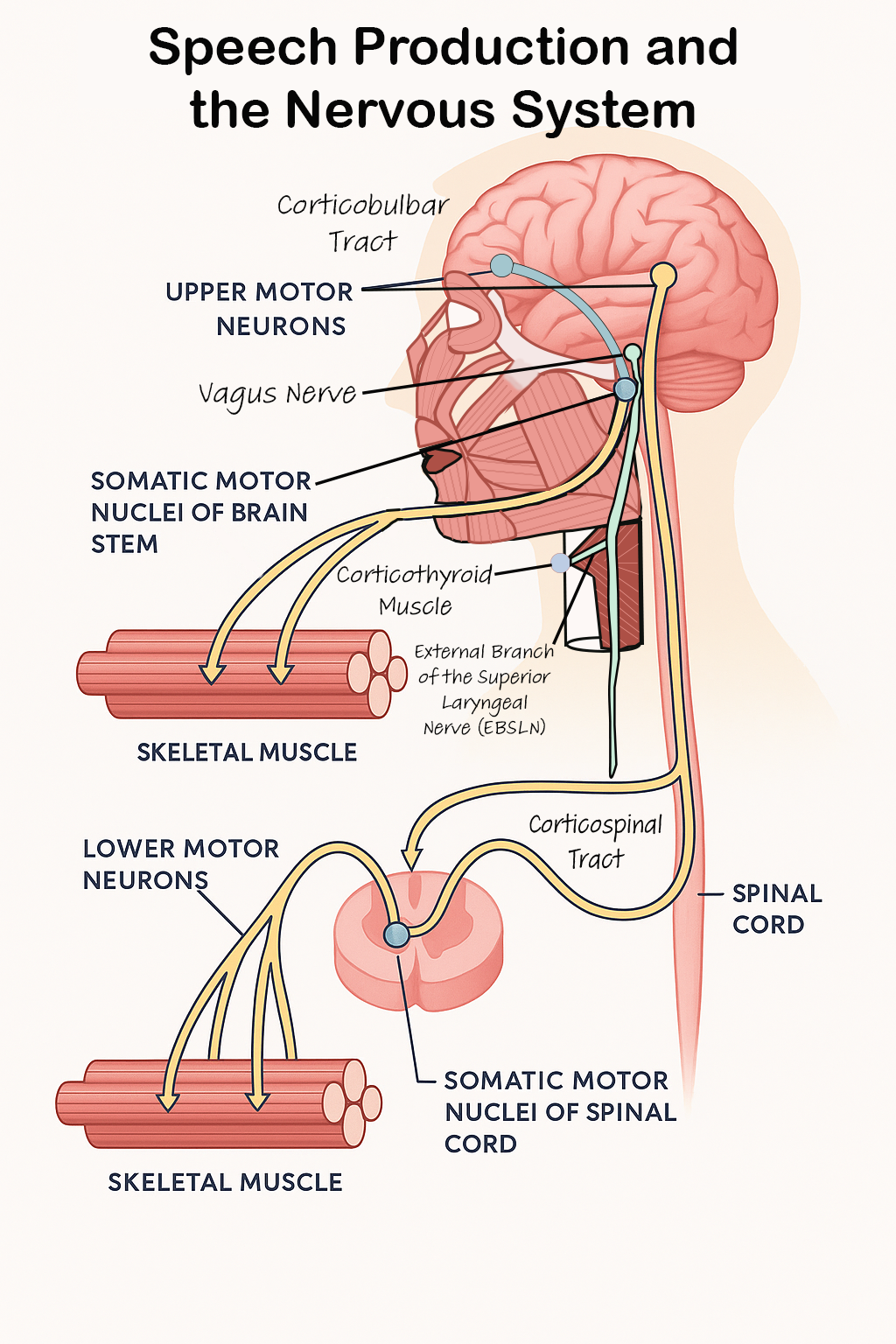
For speech to occur, the brain must send signals down the corticobulbar tract to the motor neurons that activate the muscles of the face, tongue, larynx, and jaw. One of the most crucial of these components is the external branch of the superior laryngeal nerve (EBSLN), which controls the cricothyroid muscle.
The ability exists, but it is not consistently accessible, and under prolonged stress, it can be lost.
The Three Types of Nonverbality
1. Complete Lack of Ability
The speech-motor mechanism itself is structurally or developmentally impaired, or it has been damaged over time.
The child may produce sounds, humming, or vocal stimming
Receptive language and comprehension may be intact
The physical capacity to articulate sound into words is limited
This is where regression occurs in my framework.
When the speech-motor nerves (such as the EBSLN and related pathways) are repeatedly exposed to excitotoxic stress, they can lose functional integrity. A child who once had intermittent or emerging speech may lose motor access entirely, not because the child “lost skills,” but because the nerve itself has been damaged.
This is a motor output issue, not a cognitive or linguistic one.
2. Intermittent Ability
The speech mechanism is intact, but access to speech depends on internal nervous system regulation.
Words may appear during states of calm, organization, and sensory stability
Speech access disappears during stress, overload, inflammatory response, or fatigue
The ability to speak exists, but it is not reliably accessible.
There is no loss of ability here. The variability reflects shifts in autonomic state, not cognitive change.
3. Situational Ability
The speech mechanism is functional and internally regulated, but external environment determines access.
The child may speak when alone or with trusted individuals
Speech shuts down in environments involving evaluation, unpredictability, or emotional intensity
This is often mislabeled as “selective mutism,” but the inhibition is physiological, mediated through vagus-linked stress response pathways.
The ability is present, but context determines expressionThe ability is present, but context determines access
The Critical Role of the EBSLN
The cricothyroid muscle is responsible for:
Tension and length control of the vocal folds
Pitch modulation
Precision shaping of sound into word-level articulation
This is the muscle that turns sound into speech.
The EBSLN is directly influenced by the vagus nerve, meaning that speech access is directly tied to nervous system regulation.
When this nerve pathway is disrupted, there are three primary outcomes:
1. Structural / Developmental Impairment
The nerve or muscle itself is underdeveloped or partially nonfunctional.
The child may vocalize, hum, or stim vocally
Receptive language may be intact
The physical capacity to articulate words is limited
This results in consistent nonverbal presentation.
2. Internal Stress-Mediated Motor Shutdown
The nerve and muscle are functional, but the nervous system is not regulated enough to permit fine motor control.
Words may appear during calm, low-demand, sensory-stable environments
Speech access collapses during internal stress, overload, inflammation, or fatigue
This results in intermittent speech access, often mislabeled as regression.
3. External Stress / Context Inhibition
The pathway is intact and internally regulated, but social or environmental demand triggers vagal shutdown.
The child may speak freely when alone or with trusted individuals
Speech shuts down in evaluative, unfamiliar, or unpredictable environments
This results in situational / selective nonverbality, which is physiological rather than psychological.
Why This Matters
These distinctions do not describe differences in intelligence or understanding.
They describe differences in motor access to speech.
The brain may know the word.
The child may want to speak.
The meaning may be intact.
The intention may be intact.
What is missing is reliable, regulated, fine-motor control of the speech mechanism.
This is the core of the framework:
Nonverbality is often a motor-access problem, not a language-comprehension problem. If it was, they would not be able to comprehend and utilize other forms of language, such as AAC.
A Critical Gap: These Speech-Motor Mechanisms Have Never Been Tested
Although the medical community frequently uses terms like nonverbal autism or apraxia of speech, the actual physical mechanisms required for speech production have never been evaluated in those who cannot speak.
Clinicians currently assess:
Behavior
Social communication
Receptive and expressive language
Cognitive interpretation
Speech attempts
But they do not assess:
The corticobulbar tract signals
The motor neuron activation required for speech
The function of the external branch of the superior laryngeal nerve (EBSLN)
The ability of the cricothyroid (singer’s) muscle to articulate sounds into words
The vagus-mediated regulation of fine speech-motor control
This means:
Children are labeled nonverbal without testing the system that produces speech
Motor-access issues are misinterpreted as cognitive deficits
Many children who may physically be able to speak have never received the correct evaluation
If the mechanism that produces speech is not tested, we cannot conclude that speech is not possible.
This is not a matter of opinion; it is a missing medical assessment.
Help Close This Gap
I have created a petition calling for:
Standardized testing of the EBSLN and cricothyroid function in nonspeaking individuals
Clinical evaluation of speech-motor pathway integrity
Recognition that speech access is a physical output function, not a measure of intelligence
This is a foundational step toward:
Appropriate diagnosis
Fair educational placement
Correct therapeutic support
Restoring the possibility of speech for those who have never been given the chance
Please add your name and share:
Sign the Petition to Require Speech-Motor Nerve Testing in Nonspeaking Autism
Your signature helps ensure that nonspeaking individuals are finally evaluated based on biology, not assumptions.